Foot Drop Recovery | A New Approach to Reconnecting to your Foundation
If you're unable to lift the toe end of your foot off the ground, you have a condition known as foot drop. Foot drop itself isn't typically considered a disease. Rather, it's the symptom or side effect of a bigger issue.
Foot drop is typically characterized as an abnormal gait. A case of foot drop (or "drop foot") is where the forefoot drops due to irritation, weakness, or damage to the nerves or muscles of the lower leg. Learning what causes it and how to treat it is essential to getting better.
UNDERSTANDING FOOT DROP
If you suffer from foot drop, or drop foot, you will struggle to lift up the front part of your foot. As you walk, it may even drag the ground. This usually leads to a "stepping gait" in order to compensate, which is when a person lifts their knee higher in order to bring the foot fully off the ground--as if climbing stairs. This gait may lead to your foot slamming against the floor as you put your leg down.
The cause of foot drop will influence a lot of factors associated with your case. For instance, foot drop can sometimes appear very suddenly or, in some cases, it's a condition that gradually worsens. Regardless of the cause, ignoring foot drop can lead to the underlying condition worsening with time.
Depending on the cause, foot drop can affect just one foot or both of them. You may find that the skin on your toes or top of your foot feels numb. It can be temporary or permanent. A physician will likely prescribe a brace in order to hold your foot in the proper position as you walk and move around.
WHAT CAUSES FOOT DROP?
Foot drop occurs when something happens to the muscles responsible for lifting the front of the foot. These muscles can become weak or even paralyzed due to certain conditions, including the following.
THE PERONEAL NERVE
The peroneal nerve is responsible for controlling muscles to lift the foot and injuring it is surprisingly easy at any age. The peroneal nerve brances out of the sciatic nerve. The peroneal nerve wraps around from the front of your shin to the back of your knee. It's close to the surface of the skin, which makes it easy to damage.
It's so easy to injure that you may suffer from damage while playing sports or even during childbirth. Many other activities can also put you at a higher risk of peroneal nerve damage. If you have damaged your peroneal nerve, you'll likely experience pain or numbness on the front of your shin all the way down to the top of your foot.
NERVE COMPRESSION AND INJURY
Most commonly, foot drop gets caused by compression of the peroneal nerve in the leg. For instance, damage can occur to this nerve during hip replacement or knee replacement surgery. Additionally, you may suffer from a "pinched nerve," which is an issue that occurs in the spinal region, and experience foot drop as a result.
However, other risk factors are much more common. Simply crossing your legs habitually can put you at a higher risk of foot drop because this can compress the peroneal nerve in the upper thigh region. So, too, can prolonged kneeling or squatting. Laying tile, picking berries, and other occupations that require you to do so frequently could heighten your risk.
Finally, you might experience foot drop after wearing a cast on your lower leg. If you wear a plaster cast that runs from below the knee to the top of your foot, it can put pressure on the peroneal nerve, which could lead to foot drop.
MUSCLE OR NERVE DISORDERS
People with diabetes are at a particularly high risk for nerve disorders that can cause foot drop. Additionally, muscular dystrophy is an inherited disease that can lead to foot drop. This disease causes progressively weaker muscles and, in turn, ends up weakening the muscles needed to lift the front of the foot.
Polio and Charcot-Marie-Tooth disease can also cause foot drop. This is why having any case of foot drop addressed is a necessity--it could clue you in to a much more serious condition.
BRAND AND SPINAL CORD DISORDERS
Any disorder that affects the spinal cord and/or brain can lead to foot drop. This includes ALS, or Amyotrophic Lateral Sclerosis, along with stroke, multiple sclerosis, Cerebral Palsy, and other conditions.
HOW TO TREAT FOOT DROP
Foot drop is not always permanent. The type of treatment your doctor pursues will depend on the cause of your foot drop. However, addressing the problem early will always give you a greater chance at speedy recovery.
A doctor may suggest a lightweight brace to hold the foot in its proper position. This is the most common treatment route. Alternatively, they may suggest physical therapy to help strengthen weakened muscles in the leg and foot. A physical therapist may also use a device that stimulates nerves in the leg.
In severe cases, your doctor may suggest surgery in an attempt to repair a damaged nerve or decompress it. If a case of foot drop gets diagnosed as permanent, they may suggest surgery to fuse the ankle joint to the foot or they may attempt to improve stability and gait by taking tendons from stronger muscles and transferring them into the problem area.
More commonly, doctors will suggest orthotics to address foot drop.

How Can Orthotics Help Foot Drop?
Regardless of the cause, foot drop treatment almost always involves an ankle foot orthosis (AFO) for bracing. These braces provide stability and toe clearance to help normalize the gait. They come in many different forms.
Understanding how AFOs work is essential to learning how such a product could benefit you. To do so, it's important to realize that the ankle joint sees two standard forms of motion. These motions are plantarflexion (to describe downward movement) and dorsiflexion (to describe upward movement).
Plantarflexion is the motion of the ankle joints when your toes point downward. Dorsiflexion is the motion of the ankle joins when the foot points upward. As you lift your foot off the ground, dorsiflexion needs to occur so that your toes don't drag the surface. Typically, foot drop results from weakness or paralyzation of the muscles responsible for dorsiflexion in the ankle joint.
There are multiple types of AFOs your doctor may suggest in order to address your foot drop.
ORTHOTICS WITH A SHORT LEG AND FIXED HINGE
The first is a "short leg" AFO. This design is shorter in height and features a fixed hinge. This AFO fits easily into most shoes and is fairly light. It gives you more control over your foot and it's great for foot drop and flat feet.
This AFO works to position the foot at a 90-degree angle to the leg and keep it there. This also helps to control inward foot rotation, which is common in patients who have foot drop as a result of a stroke or Charcot-Marie-Tooth.
With the fixed hinge, however, this brace does not allow for plantarflexion or dorsiflexion. That means the gait won't be as natural as some other braces may allow. Additionally, taller individuals (over six feet) will struggle with this brace because it is short.
ORTHOTICS TO ASSIST DORSIFLEXION
Some AFOs are actually designed to assist dorsiflexion and are aptly named Dorsiflexion Assist Functional AFOs. They feature a hinge reminiscent of a spring. This hinge works to promote dorsiflexion (raising the foot) when you lift your foot off the ground. In other words, it mimics the motion you would naturally make when walking.
As a result, this AFO produces a more normal gait pattern. This design is ideal for someone with mild to moderate foot drop and it can also benefit a person with a generally flat or unstable foot. However, this design typically won't work for tall people (over six feet) or people who weigh more than a certain amount (typically 225 pounds or more).
ORTHOTICS TO STOP PLANTARFLEXION
This AFO design concentrates on preventing plantarflexion in the foot. In other words, it does not allow the foot to point downward, thereby preventing toe dragging. It features a hinge to enable normal dorsiflexion. This design tends to be a bit bulkier than some others but it can be effective for those who suffer from a severe case of foot drop.
ENERGY RETURN ORTHOTICS
This AFO is perhaps one of the best designs as it is extremely lightweight in construction and provides immense control. There are usually different sub-models that vary depending on how severe a case of foot drop is. In general, an energy return AFO will use the natural flex of the AFO material itself in order to assist dorsiflexion.
Typically, you will find this type of AFO is actually constructed of carbon graphite materials. This makes them both lightweight and very good at providing dorsiflexion assistance.
TRADITIONAL ORTHOTICS
Traditional AFOs are also known as posterior leaf spring AFOs. These orthotics have been around for years and are still effective today. However, newer designs allow for more comfortable usage and are typically lighter.
With that said, a physician may still recommend a posterior leaf spring construction for someone who has both foot drop and knee instability. There are also modern designs made specifically for those with foot drop and unstable knees.
ORTHOTICS FOR UNSTABLE KNEES
Most often, a physician will suggest a "solid AFO" if you have both unstable knees and foot drop. This design will stop plantarflexion and also limit or stop dorsiflexion. If you have an unstable knee alongside a complete loss of dorsiflexion strength (or severely limited strength), this design may work best for you. While bulkier than others, it gives superior control while moving around.
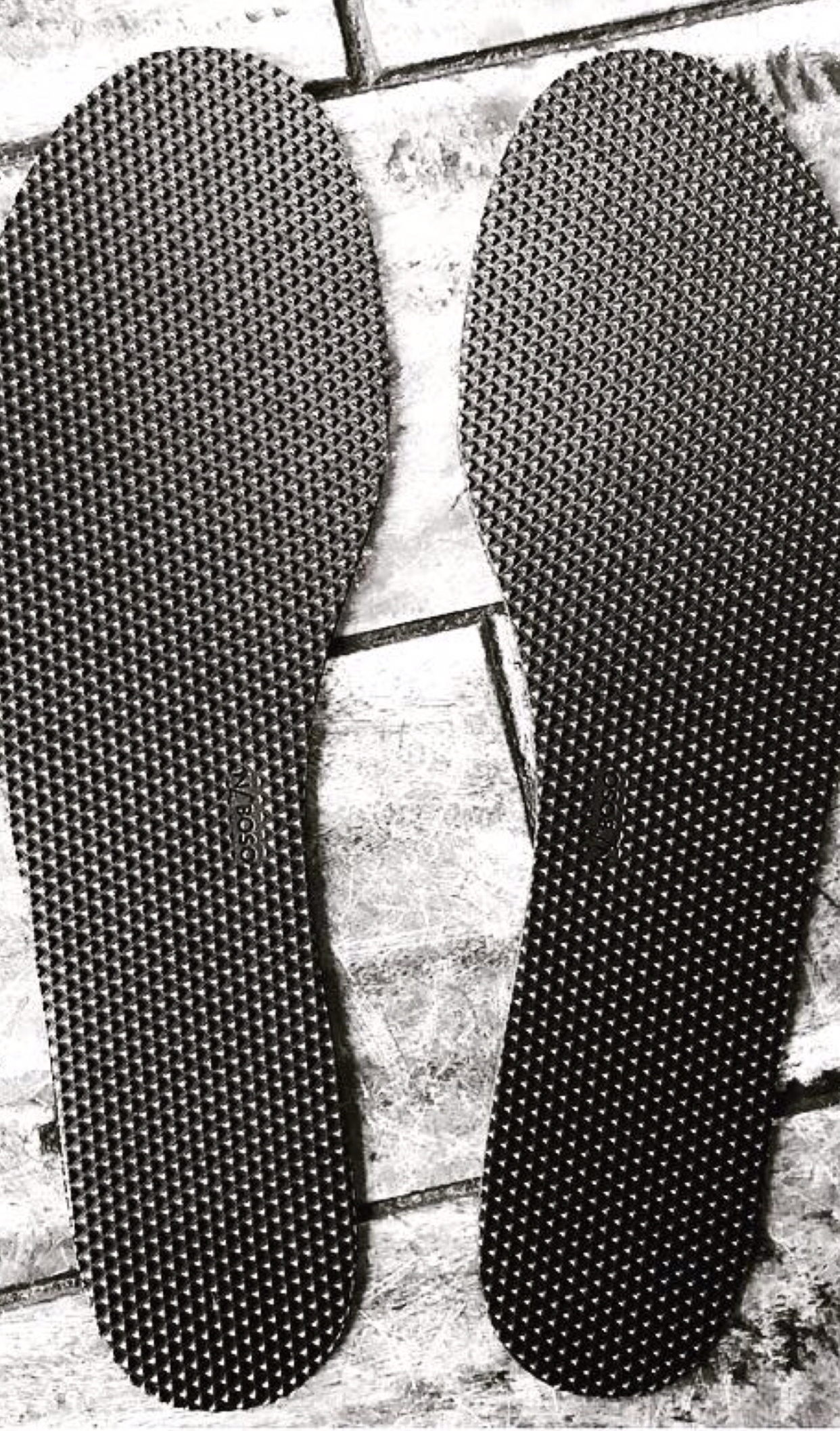
How Textured Insoles are Beneficial for Foot Drop Braces
In the likely event that your physician recommends an AFO brace, it's important to also consider the role of textured insoles as part of your treatment. This is because textured insoles add the added benefit of stimulating the skin on the bottom of the feet, brining increased neurostimulation.
Naboso™ Textured Insoles are the perfect option. Designed by Podiatrist Dr Emily Splichal, Naboso™ Textured Insoles are specifically designed to enhance proprioceptive stimulation of the feet.
WHAT IS PROPRIOCEPTIVE STIMULATION?
The skin on the bottom of your foot is home to plantar proprioceptors, which are critical to proper balance, posture, motor control, and human locomotion. However, all footwear blocks the necessary stimulation of the plantar proprioceptors to some degree. The result is a delay in communication between the ground and the nervous system. In turn, this delay can lead to poor balance, inefficient movement, and joint pain.
Proper stimulation of the plantar proprioceptors is essential to whole body wellness and, especially, to supporting healthy movement. Dr Emily Splichal designed Naboso Insoles in a way that they are able to uniquely stimulate the plantar proprioceptors.
With advanced research, Naboso Insoles have shown that they can improve gait patterns and balance. As such, Naboso Technology offer a range of insoles all of which benefit not only medical conditions and athletes, but for people of all ages.
THE BENEFITS OF MEDICAL ORTHOTICS
Properly designed orthotics are beneficial to everyone, but they play a special role in recovery or management for those suffering from foot drop and other mobility issues.
Textured insoles do more than support the foot or arch. With all of your weight bearing down on your feet, textured insoles work to alleviate pain that resonates through the foot, ankle, leg, and back. The right insert will help you to correctly align your feet and legs naturally, leading to better posture and improved balance.
By supporting the arch and heel of the foot, textured insoles help to absorb shock and distribute the immense pressure felt by your foot across your entire sole. The design of a properly fitted textured insoles will also help to prevent bunions, calluses, corns, and ulcerations thanks to the evenly distributed weight, which helps to prevent and alleviate pressure points.
All of these things typically promotes greater mobility, allowing people to stay on their feet for longer and be more active while eliminating pain and other impacts they used to suffer from when moving around.
THE IMPORTANCE OF PROPER FIT
You should never just pull a pair of generic insoles off the shelf and expect them to benefit you. The key to effective orthotics is proper construction and fit. A prefabricated option can work wonders, so long as you properly measure your foot bed to ensure that the fit is right.
If you choose an insole too small or too big, the placement of the arch support and the general shape of the insole can be uncomfortable and even worsen joint pain and other conditions. As such, you should always check size guides and ask for help when needed.
When in doubt, ask a professional for guidance and assistance in choosing the right textured insoles for your needs. If you pair your AFO with the right textured insoles, you will experience immense relief, greater stability, improved mobility, and better results as a whole.
FINDING THE RIGHT TEXTURED INSOLES
Once you have spoken to your physician about addressing your drop foot, seek their guidance in finding the appropriate AFO for your needs. With that information, you can then proceed with looking for the right textured insoles that will enable you to get the most out of your rehabilitation or management program.
If you need help finding the right textured insoles, look no further than Dr Emily Splichal andNaboso Technology. Take a few minutes and learn more Naboso™ Textured Insoles